What Is Diabetic Retinopathy?
Diabetic retinopathy (DR) is a microvascular disorder stemming from the long term effects of diabetes. As the most common cause of vision loss among working age adults, the key to avoiding blindness is timely intervention. According to the American Diabetes Association, worsening DR is most often associated with risk factors such as poor glycemic control, uncontrolled hypertension, and dyslipidemia. One’s likelihood of developing the disease is directly related to these factors along with the patient’s age and the duration of diabetes.
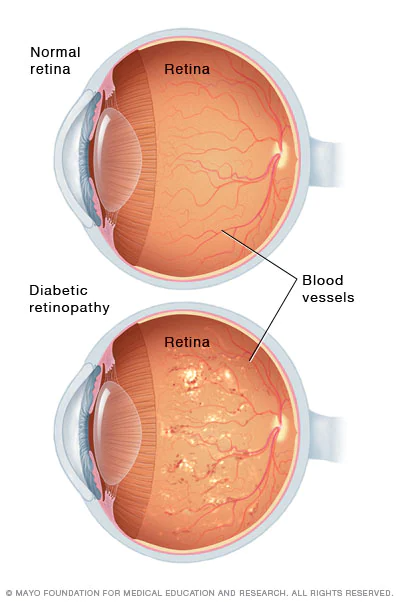
The condition presents with signs such as balloon-like swelling of the retina’s tiny blood vessels—called microaneurysms—hard exudates comprised of lipids and other material, macular edema or swelling (diabetic macular edema or DME), and in proliferative DR or PDR the formation of new blood vessels. Physician groups like the American Academy of Ophthalmology and the American Diabetes Association agree that the cornerstone of DR management is strict control of the underlying systemic conditions, ie blood glucose levels and blood pressure. The main treatment options are laser photocoagulation, intravitreal injections, and surgery. With early diagnosis and prompt management, doctors say that most patients with DR can achieve good vision.
WHAT ARE THE TYPES OF DIABETIC RETINOPATHY?
Non-proliferative Versus Proliferative Diabetic Retinopathy
There are two types of DR, nonproliferative (NPDR) and proliferative (PDR). NPDR is further categorized as mild, moderate, or severe. PDR is the most advanced form of the condition.
- Mild NPDR. In the early stage of the disease, the blood vessels leak into the retina, showing up as fluid, hemorrhages, or lipids.
- Moderate NPDR. Over time the blood vessels swell, change their shape, and become ischemic or closed off impairing blood flow. These changes can contribute to DME.
- Severe NPDR. Many more blood vessels become blocked, depriving the retina of blood. These areas secrete growth factors that signal the creation of new blood vessels.
- PDR. As the disease progresses, abnormal blood vessels proliferate, growing inside the retinal surface and into the vitreous or fluid that fills the eye. These fragile new blood vessels leak and bleed creating scar tissue that eventually causes the retina to detach from underlying tissue. Retinal detachment can result in severe vision loss.
HOW IS DIABETIC RETINOPATHY TREATED?
(1) Focal Laser Photocoagulation/Panretinal Photocoagulation. Laser therapy is a standard treatment for eyes with many types of DR. Clinical studies have shown that eyes treated in this manner had a significantly reduced risk of vision loss. Evidence from clinical trials has shown that panretinal laser photocoagulation reduces the risk of severe vision loss by at least 50%, with eyes affected with PDR experiencing the greatest benefit. Early treatment with panretinal photocoagulation can help patients before they develop characteristics that put them at high risk for vision loss.
- How photocoagulation is performed. A beam of laser light is aimed at damaged retina and small bursts of the laser’s beam seals leaking retinal vessels to reduce macular edema. To treat neovascularization, the laser beam bursts are scattered throughout the side areas of the retina. The small scars left behind from the laser lessen abnormal blood vessel growth and help bond the retina to the back of the eye, preventing retinal detachment.
- Advantages of laser surgery. Laser surgery is safe and may be performed in an ophthalmologist’s office or an outpatient clinic. If DR is detected early, laser surgery can stabilize vision loss, slowing it down, and reducing the chance of severe visual impairment even in the more advanced stages of the disease. Patients receive topical anesthesia via eye drops, and the quick procedure only lasts 15 to 20 minutes. Laser treatment can be sometimes be accomplished in as little as one visit, whereas intravitreous injections may be required chronically, over numerous visits, to adequately control DR.
- Laser treatment recovery time. Most patients are able to return to their normal activities shortly after treatment. Patients will, however, need to wear sunglasses for a period of time as the eyes will be dilated and sensitive to light. They can expect their vision to be blurry for 24 hours and they may experience some additional temporary side effects such as soreness and dark spots that will subside quickly.
- Side effects. Some possible side effects of laser treatment are a temporary mild ache of the eye or area around the eye, a “black eye” that may last for several days, blurred vision that typically lasts for a few days to a week, decreased peripheral vision, decreased color vision, decreased contrast sensitivity, temporary light flashes in your vision.
- Risks. Possible risks of treatment include but are not limited to: loss of some of vision, double vision, and a droopy eyelid.
(2) Intravitreous injections. Intravitreous injections of steroids or other drugs called anti-vascular endothelial growth factor agents may be indicated for some types of DR and are sometimes used in conjunction with laser therapy. These treatments, which take effect over weeks and months, typically need to be repeated for greatest benefit.
- Side effects and risks. After an injection patients may experience slight blurriness, redness, blood, irritation, and increased watering of the eye, all of which subside in a few days. Complications of intravitreal injections are uncommon and occur in less than 1% of the time.
(3) Vitreoretinal surgery. Vitrectomy is required for PDR when there is severe vitreous hemorrhage persisting beyond 3 months or tractional retinal detachment that is encroaching on the macula.
(4) Cryotherapy. Anterior peripheral retinal cryotherapy, treatment that involves the use of freezing or near-freezing temperatures, has been discussed as a method of preventing vitreous hemorrhage in patients with PDR.
(5) Recent and future advances. As more is learned about the protective factors at play in DR, research is looking at new therapeutic strategies that could center on stimulating endogenous mechanisms. Additional molecules have been proposed for therapeutic agents that would target alternative pathways, as current drugs have limitations. Emerging investigations are also looking at genetic strategies to slow the progression of DR in those with risk factors. The concept of cell-based treatments that could repair the retinal vasculature is also a promising area of future investigations.
(6) Alternative treatments and homeopathy. A review of herbal medicine for DR has not shown evidence that any of these compounds provide benefits.
How Much Does It Cost to Treat Diabetic Retinopathy?
In most countries, treatment will be covered by the government healthcare system. In the US, treatment options for diabetic retinopathy vary widely and can range from hundreds to several thousands of dollars. The cost of exams and treatment, however, because it is considered medically necessary this is usually covered by private insurance or Medicare. Note that vision insurance will not cover retinopathy treatment but private medical insurance usually will. The out-of-pocket costs incurred depend on the plan and provider but may include co-pays, deductibles and coinsurance costs. A 20% copayment for a single injection could range from $20 to $400 with the need for an average of 10 injections per year. For a one time laser procedure, a 20% copay could range from $200 to $400.
How Can One Protect Vision from Diabetic Retinopathy?
According to Prevent Blindness, DR can be present without symptoms, which is why it is imperative that patients with Type 1 diabetes be screened within 5 years of diagnosis, and Type 2 diabetic patients should have their first eye exam at the time of diagnosis. Diabetes patients should have annual dilated eye exams thereafter. Detecting DR early increases the odds of protecting against permanent retinal damage, vision loss, and blindness. Women with diabetes who become pregnant should have more frequent dilated eye exams. Patients with diabetes should carefully control their blood glucose levels and blood pressure to prevent or slow sight-threatening DR.

How is Diabetic Retinopathy Diagnosed?
An ophthalmologist can diagnose diabetes-related retinopathy during a comprehensive dilated exam.
He or she will check:
- Visual acuity
- Intraocular pressure to make sure there are no signs of glaucoma
- Eye muscle function
- Peripheral vision
- Pupil response and reaction
The eye doctor will use drops to dilate or widen the pupils. During this exam the doctor looks for:
- Abnormal blood vessels
- Bleeding in the center of the eye
- Growth of new blood vessels
- Retina swelling
Mayo Clinic’s Tips to Reduce the Risk of DR
- Manage diabetes through healthy eating, physical activity, and taking diabetes medications as directed.
- Monitor blood sugar level.
- Take a hemoglobin A1C test. For most people with diabetes, the A1C goal is to be under 7%.
- Keep blood pressure and cholesterol under control.
- Quit smoking.
- Pay attention to vision changes.
REFERENCES:
https://www.mayoclinic.org/diseases-conditions/diabetic-retinopathy/symptoms-causes/syc-20371611
https://doi.org/10.2337/dc16-2641
https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/diabetic-retinopathy
https://www.aao.org/preferred-practice-pattern/diabetic-retinopathy-ppp
https://www.aao.org/eye-health/diseases/what-is-diabetic-retinopathy
https://doi.org/10.2337/dc16-2641
https://www.bu.edu/eye/evidence-based-medicine/vitreo-retinal-studies/diabetic-retinopathy-study-drs/
https://www.docshop.com/education/vision/procedures/diabetic-retinopathy-surgery/recovery
https://www.retinalmd.com/retina-treatment/panretinal-photocoagulation
https://www.vision-and-eye-health.com/retinopathy-treatment.html
https://doi: 10.4103/1858-540X.118644
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5518557/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6517038/
https://www.carecredit.com/well-u/health-wellness/diabetic-retinopathy-treatment-cost-financing/
https://www.webmd.com/eye-health/ss/slideshow-eye-conditions-overview
https://adammillermd.com/2019/04/21/treatment-of-diabetic-macular-edema-does-cost-matter/
https://www.mdsave.com/procedures/photocoagulation-retinopathy-treatment/d580fdcc#
https://preventblindness.org/treatment-of-diabetic-retinopathy/
https://my.clevelandclinic.org/health/diseases/8591-diabetic-retinopathy
https://www.mayoclinic.org/diseases-conditions/diabetic-retinopathy/symptoms-causes/syc-2037161
https://www.asrs.org/patients/retinal-diseases/33/intravitreal-injections
https://medlineplus.gov/ency/article/007664.htm#
What Is Diabetic Retinopathy?
Diabetic retinopathy (DR) is a microvascular disorder stemming from the long term effects of diabetes. As the most common cause of vision loss among working age adults, the key to avoiding blindness is timely intervention. According to the American Diabetes Association, worsening DR is most often associated with risk factors such as poor glycemic control, uncontrolled hypertension, and dyslipidemia. One’s likelihood of developing the disease is directly related to these factors along with the patient’s age and the duration of diabetes.
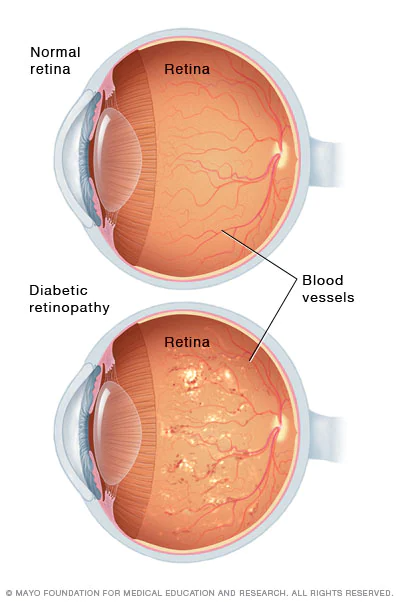
The condition presents with signs such as balloon-like swelling of the retina’s tiny blood vessels—called microaneurysms—hard exudates comprised of lipids and other material, macular edema or swelling (diabetic macular edema or DME), and in proliferative DR or PDR the formation of new blood vessels. Physician groups like the American Academy of Ophthalmology and the American Diabetes Association agree that the cornerstone of DR management is strict control of the underlying systemic conditions, ie blood glucose levels and blood pressure. The main treatment options are laser photocoagulation, intravitreal injections, and surgery. With early diagnosis and prompt management, doctors say that most patients with DR can achieve good vision.
WHAT ARE THE TYPES OF DIABETIC RETINOPATHY?
Non-proliferative Versus Proliferative Diabetic Retinopathy
There are two types of DR, nonproliferative (NPDR) and proliferative (PDR). NPDR is further categorized as mild, moderate, or severe. PDR is the most advanced form of the condition.
- Mild NPDR. In the early stage of the disease, the blood vessels leak into the retina, showing up as fluid, hemorrhages, or lipids.
- Moderate NPDR. Over time the blood vessels swell, change their shape, and become ischemic or closed off impairing blood flow. These changes can contribute to DME.
- Severe NPDR. Many more blood vessels become blocked, depriving the retina of blood. These areas secrete growth factors that signal the creation of new blood vessels.
- PDR. As the disease progresses, abnormal blood vessels proliferate, growing inside the retinal surface and into the vitreous or fluid that fills the eye. These fragile new blood vessels leak and bleed creating scar tissue that eventually causes the retina to detach from underlying tissue. Retinal detachment can result in severe vision loss.
HOW IS DIABETIC RETINOPATHY TREATED?
(1) Focal Laser Photocoagulation/Panretinal Photocoagulation. Laser therapy is a standard treatment for eyes with many types of DR. Clinical studies have shown that eyes treated in this manner had a significantly reduced risk of vision loss. Evidence from clinical trials has shown that panretinal laser photocoagulation reduces the risk of severe vision loss by at least 50%, with eyes affected with PDR experiencing the greatest benefit. Early treatment with panretinal photocoagulation can help patients before they develop characteristics that put them at high risk for vision loss.
- How photocoagulation is performed. A beam of laser light is aimed at damaged retina and small bursts of the laser’s beam seals leaking retinal vessels to reduce macular edema. To treat neovascularization, the laser beam bursts are scattered throughout the side areas of the retina. The small scars left behind from the laser lessen abnormal blood vessel growth and help bond the retina to the back of the eye, preventing retinal detachment.
- Advantages of laser surgery. Laser surgery is safe and may be performed in an ophthalmologist’s office or an outpatient clinic. If DR is detected early, laser surgery can stabilize vision loss, slowing it down, and reducing the chance of severe visual impairment even in the more advanced stages of the disease. Patients receive topical anesthesia via eye drops, and the quick procedure only lasts 15 to 20 minutes. Laser treatment can be sometimes be accomplished in as little as one visit, whereas intravitreous injections may be required chronically, over numerous visits, to adequately control DR.
- Laser treatment recovery time. Most patients are able to return to their normal activities shortly after treatment. Patients will, however, need to wear sunglasses for a period of time as the eyes will be dilated and sensitive to light. They can expect their vision to be blurry for 24 hours and they may experience some additional temporary side effects such as soreness and dark spots that will subside quickly.
- Side effects. Some possible side effects of laser treatment are a temporary mild ache of the eye or area around the eye, a “black eye” that may last for several days, blurred vision that typically lasts for a few days to a week, decreased peripheral vision, decreased color vision, decreased contrast sensitivity, temporary light flashes in your vision.
- Risks. Possible risks of treatment include but are not limited to: loss of some of vision, double vision, and a droopy eyelid.
(2) Intravitreous injections. Intravitreous injections of steroids or other drugs called anti-vascular endothelial growth factor agents may be indicated for some types of DR and are sometimes used in conjunction with laser therapy. These treatments, which take effect over weeks and months, typically need to be repeated for greatest benefit.
- Side effects and risks. After an injection patients may experience slight blurriness, redness, blood, irritation, and increased watering of the eye, all of which subside in a few days. Complications of intravitreal injections are uncommon and occur in less than 1% of the time.
(3) Vitreoretinal surgery. Vitrectomy is required for PDR when there is severe vitreous hemorrhage persisting beyond 3 months or tractional retinal detachment that is encroaching on the macula.
(4) Cryotherapy. Anterior peripheral retinal cryotherapy, treatment that involves the use of freezing or near-freezing temperatures, has been discussed as a method of preventing vitreous hemorrhage in patients with PDR.
(5) Recent and future advances. As more is learned about the protective factors at play in DR, research is looking at new therapeutic strategies that could center on stimulating endogenous mechanisms. Additional molecules have been proposed for therapeutic agents that would target alternative pathways, as current drugs have limitations. Emerging investigations are also looking at genetic strategies to slow the progression of DR in those with risk factors. The concept of cell-based treatments that could repair the retinal vasculature is also a promising area of future investigations.
(6) Alternative treatments and homeopathy. A review of herbal medicine for DR has not shown evidence that any of these compounds provide benefits.
How Much Does It Cost to Treat Diabetic Retinopathy?
In most countries, treatment will be covered by the government healthcare system. In the US, treatment options for diabetic retinopathy vary widely and can range from hundreds to several thousands of dollars. The cost of exams and treatment, however, because it is considered medically necessary this is usually covered by private insurance or Medicare. Note that vision insurance will not cover retinopathy treatment but private medical insurance usually will. The out-of-pocket costs incurred depend on the plan and provider but may include co-pays, deductibles and coinsurance costs. A 20% copayment for a single injection could range from $20 to $400 with the need for an average of 10 injections per year. For a one time laser procedure, a 20% copay could range from $200 to $400.
How Can One Protect Vision from Diabetic Retinopathy?
According to Prevent Blindness, DR can be present without symptoms, which is why it is imperative that patients with Type 1 diabetes be screened within 5 years of diagnosis, and Type 2 diabetic patients should have their first eye exam at the time of diagnosis. Diabetes patients should have annual dilated eye exams thereafter. Detecting DR early increases the odds of protecting against permanent retinal damage, vision loss, and blindness. Women with diabetes who become pregnant should have more frequent dilated eye exams. Patients with diabetes should carefully control their blood glucose levels and blood pressure to prevent or slow sight-threatening DR.

How is Diabetic Retinopathy Diagnosed?
An ophthalmologist can diagnose diabetes-related retinopathy during a comprehensive dilated exam.
He or she will check:
- Visual acuity
- Intraocular pressure to make sure there are no signs of glaucoma
- Eye muscle function
- Peripheral vision
- Pupil response and reaction
The eye doctor will use drops to dilate or widen the pupils. During this exam the doctor looks for:
- Abnormal blood vessels
- Bleeding in the center of the eye
- Growth of new blood vessels
- Retina swelling
Mayo Clinic’s Tips to Reduce the Risk of DR
- Manage diabetes through healthy eating, physical activity, and taking diabetes medications as directed.
- Monitor blood sugar level.
- Take a hemoglobin A1C test. For most people with diabetes, the A1C goal is to be under 7%.
- Keep blood pressure and cholesterol under control.
- Quit smoking.
- Pay attention to vision changes.
REFERENCES:
https://www.mayoclinic.org/diseases-conditions/diabetic-retinopathy/symptoms-causes/syc-20371611
https://doi.org/10.2337/dc16-2641
https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/diabetic-retinopathy
https://www.aao.org/preferred-practice-pattern/diabetic-retinopathy-ppp
https://www.aao.org/eye-health/diseases/what-is-diabetic-retinopathy
https://doi.org/10.2337/dc16-2641
https://www.bu.edu/eye/evidence-based-medicine/vitreo-retinal-studies/diabetic-retinopathy-study-drs/
https://www.docshop.com/education/vision/procedures/diabetic-retinopathy-surgery/recovery
https://www.retinalmd.com/retina-treatment/panretinal-photocoagulation
https://www.vision-and-eye-health.com/retinopathy-treatment.html
https://doi: 10.4103/1858-540X.118644
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5518557/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6517038/
https://www.carecredit.com/well-u/health-wellness/diabetic-retinopathy-treatment-cost-financing/
https://www.webmd.com/eye-health/ss/slideshow-eye-conditions-overview
https://adammillermd.com/2019/04/21/treatment-of-diabetic-macular-edema-does-cost-matter/
https://www.mdsave.com/procedures/photocoagulation-retinopathy-treatment/d580fdcc#
https://preventblindness.org/treatment-of-diabetic-retinopathy/
https://my.clevelandclinic.org/health/diseases/8591-diabetic-retinopathy
https://www.mayoclinic.org/diseases-conditions/diabetic-retinopathy/symptoms-causes/syc-2037161
https://www.asrs.org/patients/retinal-diseases/33/intravitreal-injections
https://medlineplus.gov/ency/article/007664.htm#

DIDN’T FIND WHAT YOU’RE LOOKING FOR?
Let us know how we can help!
DIDN’T FIND WHAT YOU
WERE LOOKING FOR?
Let us know how we can help!