What is panretinal photocoagulation?
Panretinal photocoagulation (PRP) is a laser based treatment for retinal disease, especially proliferative diabetic retinopathy. Proliferative Diabetic Retinopathy (PDR) is the growth of abnormal blood vessels on the surface of the retina leading to vision loss. PRP is performed to stop the progression of the abnormal vessel growth and stabilize further loss of vision. During the procedure, the doctor will place a multitude of laser burns across a wide area of the peripheral retina. Sometimes the procedure is broken up into two or three treatment sessions depending on the extent of the disease and the patient tolerance for the procedure.
To perform PRP, ophthalmologists use a laser attached to a slit lamp or a Laser Indirect Ophthalmoscope (LIO). Green, yellow, or red laser light is used to burn retinal tissue and stimulate the body’s healing response, reduce the retina’s demand for oxygen, and prevent the formation or progression of abnormal blood vessels.
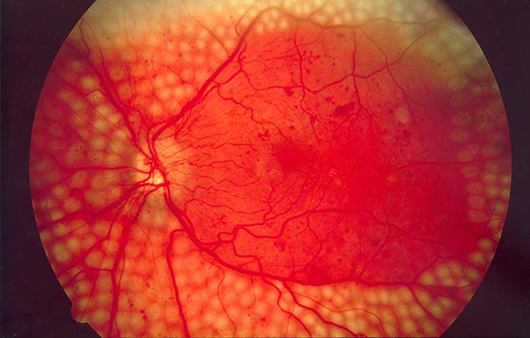 Fundus photo showing scatter laser surgery for diabetic retinopathy. EyeWiki, 17 December 2022, https://eyewiki.aao.org/Panretinal_Photocoagulation
Fundus photo showing scatter laser surgery for diabetic retinopathy. EyeWiki, 17 December 2022, https://eyewiki.aao.org/Panretinal_Photocoagulation
What eye conditions does PRP laser therapy treat?
PRP is primarily used to treat ischemic diseases of the retina including:
Diabetic Retinopathy
Diabetic retinopathy is the most common reason for a PRP procedure. Diabetic Retinopathy is characterized by two types: non-proliferative and proliferative. In non-proliferative diabetic retinopathy, the existing vascular structure of the retina may have microaneurysms that leak fluid and blood into the vitreous or have a swelling of the macula causing a loss of vision. In proliferative diabetic retinopathy, abnormal vessels begin to grow across the retina. This is called neovascularization. These vessels can bleed into the vitreous of the eye causing moderate to severe changes in vision.
Retinopathy of Prematurity (ROP)
Retinopathy of prematurity is a condition in premature infants where the growth of abnormal blood vessels dislocate the retina and can lead to permanent blindness. Similar to proliferative diabetic retinopathy treatment with a laser, PRP can help stop the progression of the vessels and limit the damage caused by ROP.
How does PRP laser work?
According to the American Academy of Ophthalmology’s (AAO) knowledge base, standard Diabetic Retinopathy Study (DRS) protocol for lasers specifies burns ranging approximately from 200μ to 500μ in size, delivered via pulse durations of 100 milliseconds at 200-250 mW of power. DRS recommends that physicians create cooler, gray burns and avoid dense, white burns. Other, specific protocols may include:
Protocols and Guidelines
Long-Duration Typical Treatment (Conventional)
The oldest and most conventional form of PRP, associated with the highest levels of patient discomfort. Burns are delivered individually and procedure durations are longer.
Short-Duration Treatment
Typically delivered via pattern scanning laser, multiple burns are placed at a time, reducing overall treatment time and increasing patient comfort.
Subthreshold Diode Micropulse
First used to treat diabetic macular edema (DME), subthreshold diode micropulse (SDM) uses a laser that is “pulsed” at an incredibly fast rate to treat ocular tissue without leaving visible burns. According to the AAO, SDM can be used to treat conditions associated with PRP, although it is still considered experimental.
Procedure
Prior to PRP, the patient is given eye drops to dilate the pupils. Local anesthetic may be applied depending on the patient’s specific anatomical condition. Patients remain awake during the procedure.
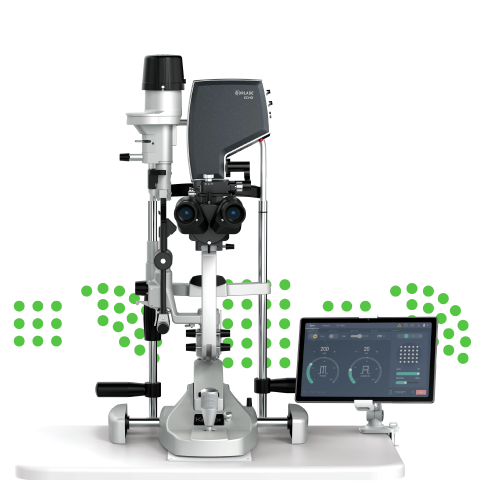
Slit Lamp Procedure
The patient is seated at a slit lamp and a contact lens is placed on the eye in order for the doctor to see a magnified image of the retina. The doctor may ask the patient to look in different directions during the procedure. The procedure may take from 5-20 minutes to complete.
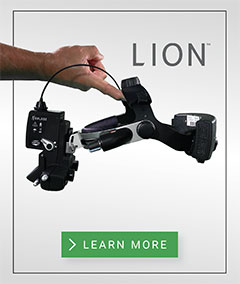
Laser Indirect Ophthalmoscope Procedure
The patient is in a supine position. The doctor uses a non-contact lens to magnify the view of the retina. The doctor may ask the patient to look in different directions during the procedure. The procedure may take from 5-20 minutes to complete.
Panretinal Photocoagulation complications and side effects
PRP is a safe and established procedure, but side effects and complications may occur. These side effects may include:
- Choroidal effusions
- Exudative retinal detachments
- Macular edema
- Visual field deficits
- Night vision defects
Although some of these side effects are considered serious (i.e., detachments and edema), the risk of untreated, progressive retinal disease or glaucoma means treatment is essential for long-term outcomes. Pattern laser, micropulse, and other ophthalmic laser modalities that reduce treatment time and/or ensure subvisible treatment may reduce the risk of side effects.
Conclusion
PRP is a well-established and effective way to prevent the progression of proliferative diabetic retinopathy and other ischemic eye disease. Today, laser technology continues to advance, with ophthalmic laser manufacturers developing new and helpful ways to improve treatment efficiency. The recently-launched Norlase ECHO, for instance, allows ophthalmologists to deliver PRP treatment with pattern technology and a high degree of precision. Its unprecedented portability, proprietary Micro-Electro-Mechanical System (MEMS) technology, and attractive price point make PRP treatment with a pattern laser more accessible to all ophthalmologists.
FAQ
When is PanRetinal Photocoagulation used in treatment?
PRP is generally used to prevent the progression of abnormal vascular growth in the retina and stabilize or prevent further vision loss.
Is PRP laser painful?
PRP can be felt by patients but doctors will take steps to minimize discomfort during the procedure. Most PRP treatments utilize green or yellow laser light which result in the patient also being temporarily affected by the flashes of light during treatment. This usually resolves in a few hours after treatment.
Does PRP affect vision?
Following PRP, a patient’s vision will likely be affected for several days or weeks. Blurred or distorted vision is common, and may get better with time. However, in many cases some vision may not return to pre-treatment levels because the purpose of the treatment is to prevent catastrophic vision loss and stabilize the progression of the disease.
What laser is used for PRP?
Today, green, yellow or red wavelength lasers are typically used for PRP.
Does PRP laser surgery cure diabetic retinopathy?
Laser surgery does not cure diabetic retinopathy, but can help control the progression of severe vision loss.
What is panretinal photocoagulation?
Panretinal photocoagulation (PRP) is a laser based treatment for retinal disease, especially proliferative diabetic retinopathy. Proliferative Diabetic Retinopathy (PDR) is the growth of abnormal blood vessels on the surface of the retina leading to vision loss. PRP is performed to stop the progression of the abnormal vessel growth and stabilize further loss of vision. During the procedure, the doctor will place a multitude of laser burns across a wide area of the peripheral retina. Sometimes the procedure is broken up into two or three treatment sessions depending on the extent of the disease and the patient tolerance for the procedure.
To perform PRP, ophthalmologists use a laser attached to a slit lamp or a Laser Indirect Ophthalmoscope (LIO). Green, yellow, or red laser light is used to burn retinal tissue and stimulate the body’s healing response, reduce the retina’s demand for oxygen, and prevent the formation or progression of abnormal blood vessels.
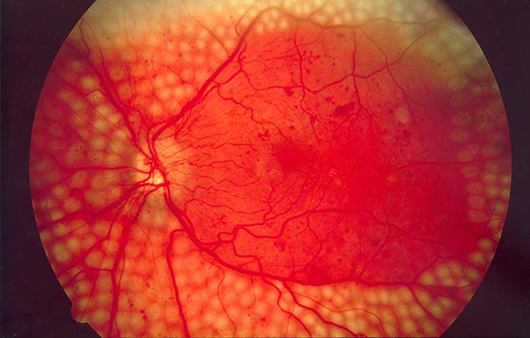 Fundus photo showing scatter laser surgery for diabetic retinopathy. EyeWiki, 17 December 2022, https://eyewiki.aao.org/Panretinal_Photocoagulation
Fundus photo showing scatter laser surgery for diabetic retinopathy. EyeWiki, 17 December 2022, https://eyewiki.aao.org/Panretinal_Photocoagulation
What eye conditions does PRP laser therapy treat?
PRP is primarily used to treat ischemic diseases of the retina including:
Diabetic Retinopathy
Diabetic retinopathy is the most common reason for a PRP procedure. Diabetic Retinopathy is characterized by two types: non-proliferative and proliferative. In non-proliferative diabetic retinopathy, the existing vascular structure of the retina may have microaneurysms that leak fluid and blood into the vitreous or have a swelling of the macula causing a loss of vision. In proliferative diabetic retinopathy, abnormal vessels begin to grow across the retina. This is called neovascularization. These vessels can bleed into the vitreous of the eye causing moderate to severe changes in vision.
Retinopathy of Prematurity (ROP)
Retinopathy of prematurity is a condition in premature infants where the growth of abnormal blood vessels dislocate the retina and can lead to permanent blindness. Similar to proliferative diabetic retinopathy treatment with a laser, PRP can help stop the progression of the vessels and limit the damage caused by ROP.
How does PRP laser work?
According to the American Academy of Ophthalmology’s (AAO) knowledge base, standard Diabetic Retinopathy Study (DRS) protocol for lasers specifies burns ranging approximately from 200μ to 500μ in size, delivered via pulse durations of 100 milliseconds at 200-250 mW of power. DRS recommends that physicians create cooler, gray burns and avoid dense, white burns. Other, specific protocols may include:
Protocols and Guidelines
Long-Duration Typical Treatment (Conventional)
The oldest and most conventional form of PRP, associated with the highest levels of patient discomfort. Burns are delivered individually and procedure durations are longer.
Short-Duration Treatment
Typically delivered via pattern scanning laser, multiple burns are placed at a time, reducing overall treatment time and increasing patient comfort.
Subthreshold Diode Micropulse
First used to treat diabetic macular edema (DME), subthreshold diode micropulse (SDM) uses a laser that is “pulsed” at an incredibly fast rate to treat ocular tissue without leaving visible burns. According to the AAO, SDM can be used to treat conditions associated with PRP, although it is still considered experimental.
Procedure
Prior to PRP, the patient is given eye drops to dilate the pupils. Local anesthetic may be applied depending on the patient’s specific anatomical condition. Patients remain awake during the procedure.
Slit Lamp Procedure
The patient is seated at a slit lamp and a contact lens is placed on the eye in order for the doctor to see a magnified image of the retina. The doctor may ask the patient to look in different directions during the procedure. The procedure may take from 5-20 minutes to complete.
Laser Indirect Ophthalmoscope Procedure
The patient is in a supine position. The doctor uses a non-contact lens to magnify the view of the retina. The doctor may ask the patient to look in different directions during the procedure. The procedure may take from 5-20 minutes to complete.
Panretinal Photocoagulation complications and side effects
PRP is a safe and established procedure, but side effects and complications may occur. These side effects may include:
- Choroidal effusions
- Exudative retinal detachments
- Macular edema
- Visual field deficits
- Night vision defects
Although some of these side effects are considered serious (i.e., detachments and edema), the risk of untreated, progressive retinal disease or glaucoma means treatment is essential for long-term outcomes. Pattern laser, micropulse, and other ophthalmic laser modalities that reduce treatment time and/or ensure subvisible treatment may reduce the risk of side effects.
Conclusion
PRP is a well-established and effective way to prevent the progression of proliferative diabetic retinopathy and other ischemic eye disease. Today, laser technology continues to advance, with ophthalmic laser manufacturers developing new and helpful ways to improve treatment efficiency. The recently-launched Norlase ECHO, for instance, allows ophthalmologists to deliver PRP treatment with pattern technology and a high degree of precision. Its unprecedented portability, proprietary Micro-Electro-Mechanical System (MEMS) technology, and attractive price point make PRP treatment with a pattern laser more accessible to all ophthalmologists.
FAQ
When is PanRetinal Photocoagulation used in treatment?
PRP is generally used to prevent the progression of abnormal vascular growth in the retina and stabilize or prevent further vision loss.
Is PRP laser painful?
PRP can be felt by patients but doctors will take steps to minimize discomfort during the procedure. Most PRP treatments utilize green or yellow laser light which result in the patient also being temporarily affected by the flashes of light during treatment. This usually resolves in a few hours after treatment.
Does PRP affect vision?
Following PRP, a patient’s vision will likely be affected for several days or weeks. Blurred or distorted vision is common, and may get better with time. However, in many cases some vision may not return to pre-treatment levels because the purpose of the treatment is to prevent catastrophic vision loss and stabilize the progression of the disease.
What laser is used for PRP?
Today, green, yellow or red wavelength lasers are typically used for PRP.
Does PRP laser surgery cure diabetic retinopathy?
Laser surgery does not cure diabetic retinopathy, but can help control the progression of severe vision loss.

DIDN’T FIND WHAT YOU’RE LOOKING FOR?
Let us know how we can help!
DIDN’T FIND WHAT YOU
WERE LOOKING FOR?
Let us know how we can help!